Anterior Cruciate Ligament (ACL) reconstruction

“I could not have been treated any better in all aspects of my knee surgery. My Surgeon Mr Charles Willis-Own was amazingly supportive and Did a fantastic job of my surgery and the whole team at The Nuffield treated me with kindness and repect and made me feel I was in very safe hands
What is the ACL?
The ACL is a strong ligament that runs diagonally through the middle of your knee. It stabilises the knee and stops it giving way, especially when you twist or pivot. As well as its mechanical role, it serves as a very important sensor to contribute to balance and joint position sense (proprioception).
The ACL is one of the most commonly injured ligaments. It’s usually torn when you slow down very quickly while turning or sidestepping at the same time. You’re more likely to injure your ACL if you play certain sports, particularly football, netball or skiing, but many people rupture their cruciate ligaments in other ways.
The images below show what a normal ACL looks like, as compared with a torn or ruptured ACL.


What is ACL Reconstruction?
If you have a torn ACL (torn knee ligament) it will generally not heal itself, and often can’t be repaired. This can leave the knee unstable and prone to giving way, particularly with twisting sports, but even with just day to day life. If something can’t be repaired we have to make a new one – and this is what ACL reconstruction is.
ACL reconstruction involves replacing your torn ligament with a graft. The graft is usually taken from a tendon in another part of your knee, usually the Hamstrings tendons on the inside of the knee, sometimes part of the patellar tendon, or alternatively allograft or synthetic ligaments.
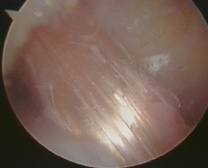
This is what a reconstructed ACL looks like when it is fresh.
Preparing for an anterior cruciate ligament reconstruction
It is best to have an ACL reconstruction either within 48 hours when the injury is fresh, or between three and eight weeks after your injury. This allows any swelling to go down but is before you have had any more injuries. In reality, many patients come months or years after the original injury and this is fine too.
I may ask you to have physiotherapy before the surgery for “prehabilitation”. This is to make sure you can move your knee as fully as possible before your operation, to teach you the exercises you will need after the surgery and to get the muscles around your knee in best possible shape to have the surgery. Importantly we can’t go ahead with the surgery unless you can get the knee fully straight and fully bent. The stronger you are coming into the op the faster you will recover.
I will discuss with you what will happen before, during and after your procedure. This is your opportunity to understand what will happen, and you can help yourself by preparing questions to ask about the risks, benefits and any alternatives to the procedure. This will help you to be informed, so you can give your consent for the procedure to go ahead, which you will be asked to do by signing a consent form.
If you smoke, you MUST stop, as smoking increases your risk of getting a chest and wound infection, which can slow your recovery. Smokers get a worse outcome and a higher failure rate. Some studies show a 7 times increased failure rate!
What happens during an anterior cruciate ligament reconstruction
ACL reconstruction is usually done with general anaesthetic but can be done with a spinal anaesthetic. If you’re having a general anaesthetic, you will be asked to follow fasting instructions. This means not eating or drinking, typically for about six hours beforehand. However, it’s important to follow the anaesthetist’s advice. I usually use a nerve block too, this means that the area we operate on will be numb for about 24 hours after the op and it means you don’t feel much pain at all.
Once you are asleep I’ll examine your knee to check how badly your ligament is torn and whether any other tendons or ligaments have been damaged. Then I will take out the hamstrings tendon that will be used to make the new ACL. This can be sore afterwards and feels like a badly pulled hamstring. Within 6 weeks of the surgery, the body recovers and regenerates a new cord where the tendon used to be.
I will then make a number of keyhole cuts in the skin over your knee and insert the camera and other surgical instruments into your knee through these cuts. I’ll deal with any other problems in the knee at this stage; torn cartilages will be trimmed or repaired. Damage to the articular surface will be treated too. It is often these factors that determine what restrictions you have to follow after the surgery, and how good the end result is.
I then need to make a tunnel through your upper shinbone and lower thigh bone, and put the graft into the tunnel, attach it to the bones and fix it in place. I’ll stitch you up and put on waterproof adhesive dressing. A large bandage is then wrapped around the leg to control the swelling. I like to leave a pipe and a bottle (called a surgical drain) coming out of the knee so that any bleeding goes into the bottle, not the knee. We discard this after a few hours, but it really helps because you don’t start your recovery with a knee full of blood!
The operation usually lasts about an hour or so.
What to expect afterwards
You will need to rest until the effects of the anaesthetic have passed and will need pain relief to help with any discomfort as the anaesthetic wears off. It is best to keep your leg elevated as much as possible. I like to keep you in hospital for about 8 hours, so if the op is in the morning you can go home the same day but if it’s after lunch then we will need you to stay overnight.
You will be given painkillers to take home. Ice packs and elevation are also helpful in the first few days. If you can get a GameReady (you can hire these from physios or from a number of online companies) or a cryocuff, these REALLY help.
You will be encouraged to get up, put weight through your knee and move it as soon as you’re able to after your surgery and the physios will help you do this. You will need to arrange for someone to drive you home. You should try to have a friend or relative stay with you for the first 24 hours after your operation.
Once you are home take it easy and elevate the leg to control the swelling. You can walk around and most people need crutches for 7-14 days, but there is no rule. The large bandage can be removed at 48 hours. The waterproof adhesive dressing will be bloodstained and appear dirty. These have been put on in a sterile environment so they should be left alone for 2 weeks, not changed. I will give you spares, but these are to go on over the top. Don’t take off the original ones.
You will also see a physiotherapist who will give you some exercises to do while you recover. The amount of physiotherapy you need varies, so follow your tailored advice. Good physiotherapy is vital to the success of this operation. Getting a good result is about one third what happens in the operating room and two thirds what happens in physio! Your job in the first 2 weeks is simple; we need to get the knee moving from 0-90 degrees (fully straight and bending to a right angle) by day 14.
I’ll check on you at about 2 weeks, 6 weeks and six months to make sure everything goes perfectly. In the unlikely event that there are any problems I’ll be there for you – always come straight to me.

It usually takes about a year to make a full recovery from ACL reconstruction but this varies between individuals, so it’s important to follow your surgeon’s advice. If you have a desk job, you may be able to go back to work three to four weeks after your operation. It may take up to six months if you have an active job, and nine months to a year to return to professional level sport safely.
What are the risks?
As with every procedure, there are some risks associated with ACL reconstruction. Fortunately, these are rare:
- Anaesthetic problems
- Infection
- Bleeding
- Scars
- Blood clots (DVT / PE)
- Stiffness
- Swelling
- Pain from the donor site for the graft (hamstrings pain)
- Mechanical symptoms – clicking and crunching due to scar tissue
- Graft re-rupture (about a 6% chance) or ongoing instability (graft stretching)
- Ongoing instability (the knee still giving way)
- Damaging an important blood vessel or nerve (very rare but very serious and I have heard horror stories of this leading to amputation in the hands of inexperienced surgeons)
- Having to take the tendons from the opposite leg
- Need for more surgery
Mr Willis-Owen will discuss these with you prior to surgery. If you have any questions it may be helpful to note them down to remind you to ask him.
Book a consultationFrequently asked questions
In recent years lots of research has been taking place to try and improve the results of anterior cruciate ligament reconstruction surgery. We have found out that in many injured knees a different structure called the anterolateral ligament (ALL) is also ruptured. This is a little band that sits on the outside of the knee and is really important in rotational stability. If we ignore this then the likelihood of re-injuring the ACL graft is higher and the chances of returning to sport seem to be lower because the knee can still give way.
There are two different techniques in widespread use for dealing with this problem and knee surgeons love to argue about whose technique is best!
The first technique which happens to be one I have developed over the years (and prefer) is called anterolateral ligament reconstruction or ALL recon. This involves making a new little band where the ruptured ligament was either with a piece of synthetic material or one of your tendons. It's fixed in the right spot with two small plastic fixation devices which cause no trouble and stay there forevermore. It can be done through two 1 cm scars on the outside of the knee. If we use the synthetic material then there is no cost to you in terms of having to take other bits of your body to reconstruct the ALL. I've done hundreds to date so far, trained a number of other surgeons and have been really pleased and delighted with the results. The published results are excellent.
The Alternative is called LET or lateral extra-articular tenodesis. This involves making a cut of about 6 to 10 cm on the outside of the knee and taking about one-third of the iliotibial band at that level, then re-routing this and fixing it with a staple or other fixation device onto the side of the thigh bone. Enthusiasts for this procedure say that it recreates the anatomy of the ALL better, but it definitely comes with more of a cost and there is plenty of research showing that the ITB is also really important in rotational stability of the knee. No one has really quantified or looked at the damage caused by taking a strip from the ITB. In my mind, it needs to be proven to be superior before the increased damage caused by the surgery can be justified.
Without a doubt, both techniques can achieve very good results with the knee feeling much more solid and stable. I prefer the ALL because it only takes 10 minutes, it causes minimal damage and scarring, and it doesn't rely on harvesting more parts of your already injured knee.
There are some studies just beginning trying to compare the two techniques head-to-head but because there are a lot of variables and only a few ACL reconstructions fail it will take quite some time to know which is superior.
Please take the time to read Mr Willis-Owen's ACL reconstruction information booklet. We can also provide further information on some of the latest advances that Mr Willis-Owen may use to get you the best result such as single tendon ACL reconstruction, and Antero-lateral ligament augmentation (ALL).